I. Introduction
The distal humerus consists of the medial and lateral columns, which include the epicondyles and condyles.
II. Surgical Procedure
Distal humerus fractures are caused by direct trauma (e.g., falls) or indirect forces (e.g., twisting or muscle pull).
III. Post-op Rehabilitation
The AO classification divides distal humerus fractures into three main types: A , B , and C .
IV. Study Results
Surgical treatment follows AO principles: anatomical reduction, stable fixation, and early rehabilitation.
V. Case Report
Locking plates offer superior biomechanical stability, particularly in osteoporotic bone.
VI. Discussion
CZMEDITECH offers three models: extraarticular (01.1107), lateral (5100-17), and medial (5100-18) plates.
VII. Conclusion
Surgical treatment follows AO principles: anatomical reduction, stable fixation, and early rehabilitation.
Distal tibial fractures are common, and traditional treatments have limitations
Distal tibial fractures are a common type of lower limb fracture. Traditional treatments such as locking plates and antegrade intramedullary nails each have their drawbacks. Locking plates may cause postoperative infections or soft tissue necrosis, prolonging recovery; although antegrade nails are minimally invasive, they may damage the knee joint, cause pain, and carry risks of inadequate fixation or malalignment, hindering recovery.
Locking plates:
Significant soft tissue damage, high infection rate, long recovery
Antegrade nails:
Risk of knee joint injury, inadequate fixation, prone to malalignment
New solution: Distal Tibial Nail (DTN)
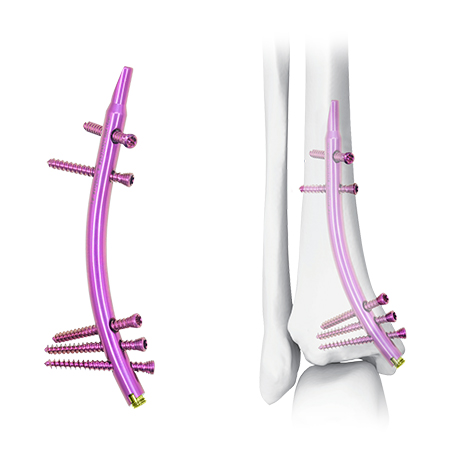
A novel treatment option—Distal Tibial Nail (DTN)—offers a new perspective for managing distal tibial fractures with its unique retrograde design.
Retrograde insertion design provides a new approach

Patient positioning and reduction preparation
The patient is placed in the supine position. Displaced fractures should be reducible manually; if necessary, use reduction forceps to assist before inserting the DTN. If there is an accompanying fibular fracture, proper fibular alignment can aid tibial reduction. Fibular shaft fractures may be stabilized with intramedullary nails. For fractures around the ankle, anatomical reduction and fixation of the fibula should precede tibial reduction to avoid malalignment. In open fractures with existing external fixation, the nail can be inserted while maintaining the fixator to achieve reduction.
Supine position, use reduction forceps if needed
Prioritize fibular fracture management to ensure accurate tibial reduction
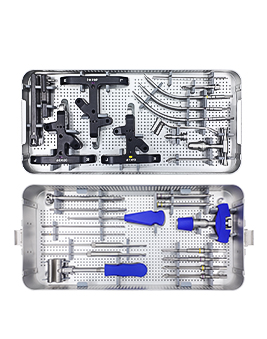
DTN insertion procedure
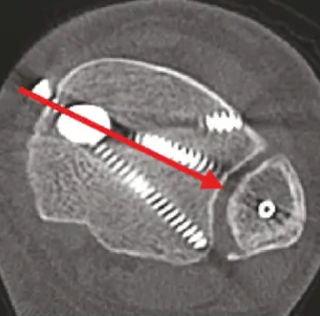
A 2–3 cm longitudinal incision is made at the tip of the medial malleolus to expose the superficial deltoid ligament. A guide pin is inserted at or slightly medial to the tip of the malleolus (Fig. 2a), 4–5 mm from the articular surface. Lateral view shows insertion via the intercondylar groove (Fig. 2b), avoiding damage to the posterior tibialis muscle. Separate the superficial deltoid ligament, then use a reamer to enlarge the medullary canal up to the metaphyseal region (Fig. 2c). Remove cancellous bone near the proximal medial cortex to insert the nail (Fig. 2d). Insert a trial nail to confirm DTN size (Fig. 2e). Avoid hammering or excessive twisting to prevent iatrogenic medial malleolar fracture. Adjust nail depth to ensure distal screws do not enter the ankle joint or fracture site. Fixation is achieved with interlocking screws proximally and distally.
Incision:
Longitudinal cut at the medial malleolus tip
Guide pin positioning:
4–5 mm from the joint surface
Reaming & trial nail:
Ream up to the metaphysis, confirm nail size
Nail insertion:
Avoid hammering, adjust depth to protect joint
Fixation:
Interlocking screws proximally and distally







Immediate ankle joint mobility and foot-to-floor contact is allowed postoperatively
Non-weight bearing for 4–6 weeks
Progress to full weight-bearing between weeks 8–12, while monitoring callus formation and painAnkle joint activity starts immediately after surgery
Avoid weight-bearing for 4–6 weeks
Gradual transition to full weight-bearing at 8–12 weeks
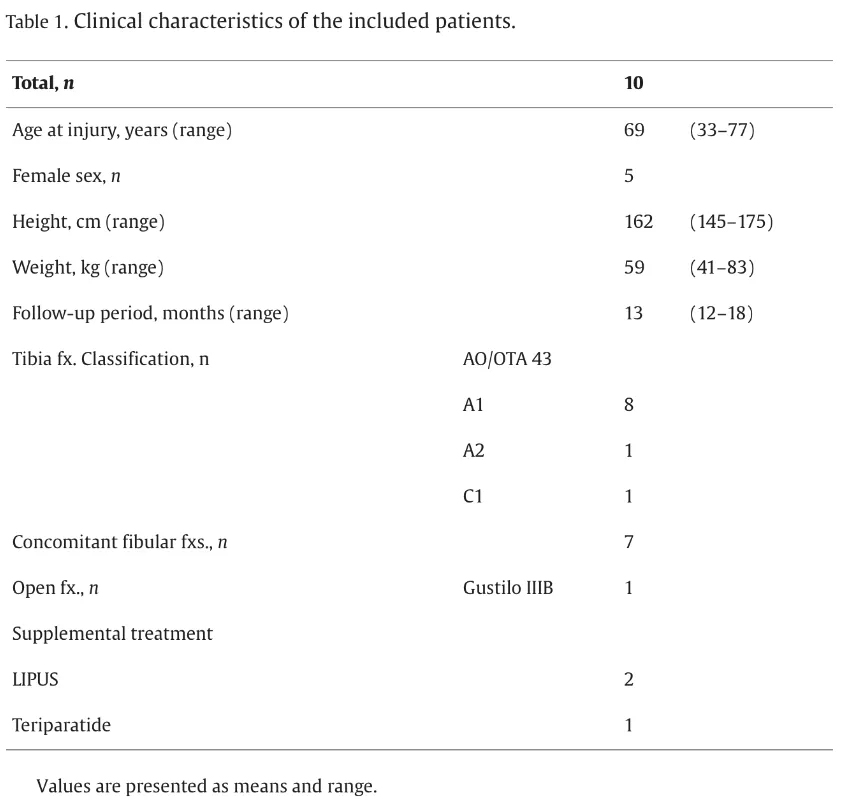
Follow-up of 10 patients
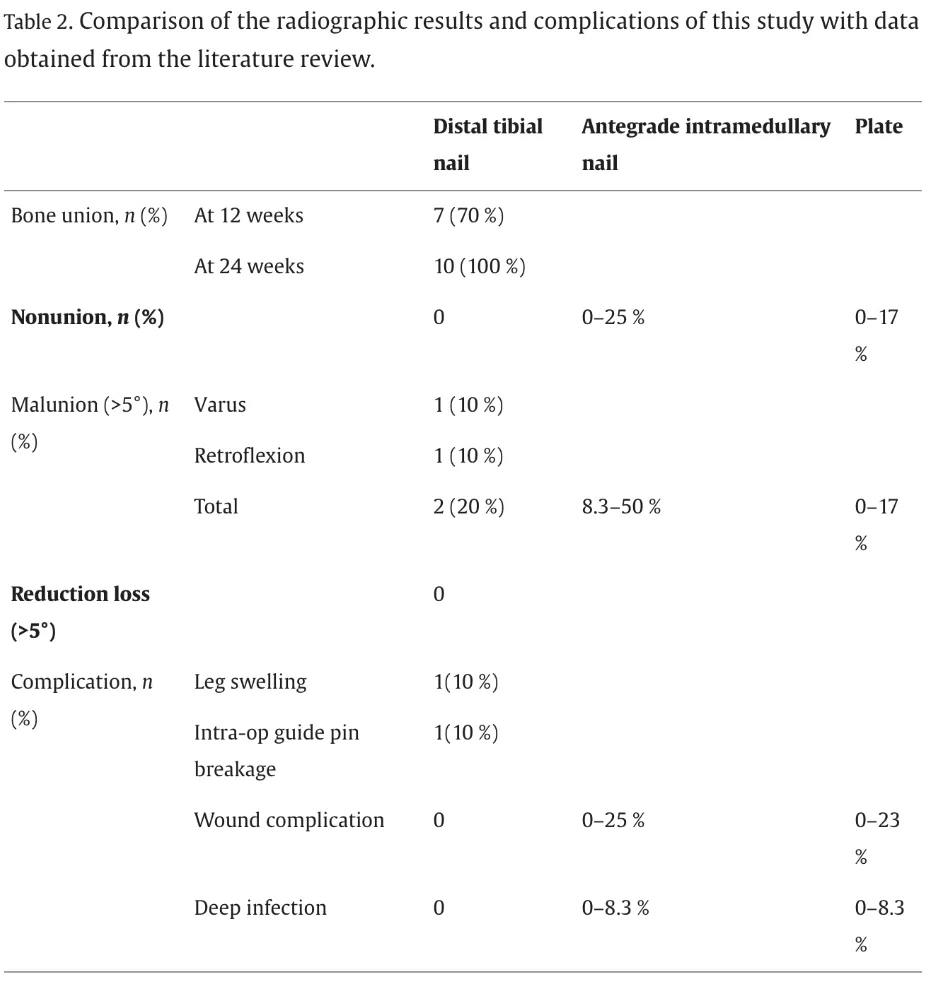
A study followed 10 patients (Table 1). By 3 months post-op, 7 cases had healed; all patients achieved healing within 6 months. One case each of varus and recurvatum deformities occurred. No loss of reduction, infection, implant-related complications, or iatrogenic injuries were observed (Table 2).
7 cases healed within 3 months; all healed by 6 months
2 mild deformities (1 varus, 1 recurvatum)
No infections, implant complications, or reduction loss
69-year-old male patient
Fracture type:
Transverse tibial fracture + fibular fracture
Complication:
Soft tissue crush injury
Post-op:
Only 6 small incisions, complete healing within 1 year
Figures 3 & 4:
Radiographic and postoperative recovery images






Indications for DTN
This study included AO 43-A and C1 fractures; C2 was also considered. DTNs are available in lengths of 7 mm and 8 mm, which determine the placement of proximal interlocking screws. Fractures located 2–9 cm above the articular surface are ideal candidates for DTN fixation. Indications can potentially be extended to AO 42 fractures.
Applicable to AO 43-A, C1, consider expanding to C2 and 42
Best outcomes for fractures 2–9 cm from the joint surface
Biomechanical Stability
Retrograde nails have superior axial and rotational stiffness compared to medial locking plates and antegrade nails. Greenfield et al. conducted biomechanical testing showing that using two distal screws in the DTN achieved 60–70% of the compressive stiffness and 90% of the torsional stiffness compared to three screws. DTN minimized fracture fragment movement under load. In 3 cases that didn’t heal within 3 months, factors included soft tissue damage, medullary expansion, fracture location, and osteoporosis. Since DTNs come in only three sizes and distal fixation is limited to three screws, they may provide insufficient stability in wide canals or osteoporotic bone. Early weight-bearing should be approached with caution in such cases.
Superior to locking plates and antegrade nails
Recommended fixation strategy: 2 proximal + 3 distal screws
Advantages of DTN
Compared to locking plates, intramedullary nails cause less soft tissue damage, particularly suitable for elderly patients and those with severe soft tissue injuries from high-energy trauma. In this study, DTNs were inserted through only six small incisions, with no soft tissue complications. The procedure does not require knee flexion, reducing the risk of reduction loss and making it suitable for patients with limited knee motion (e.g., knee arthritis or post-TKA).
Minimally invasive, ideal for elderly and high-energy trauma patients
No knee flexion needed, suitable for limited knee mobility
Surgical Risks and Precautions
Risks include injury to the posterior tibialis muscle and medial malleolar fracture. Medial malleolar fractures may be treated with tension band wiring, plating, or external fixation.
Care must be taken to avoid screw penetration into the fibular notch. The positioning device may cause posterior rotation of the DTN due to its weight; adjust the second screw to point toward the fibula (Fig. 4c).Potential complications:
Posterior tibialis injury, medial malleolar fracture
Management:
Tension band, plating, or external fixator
Screw direction and positioning device weight require intraoperative attention
Clinical Comparison
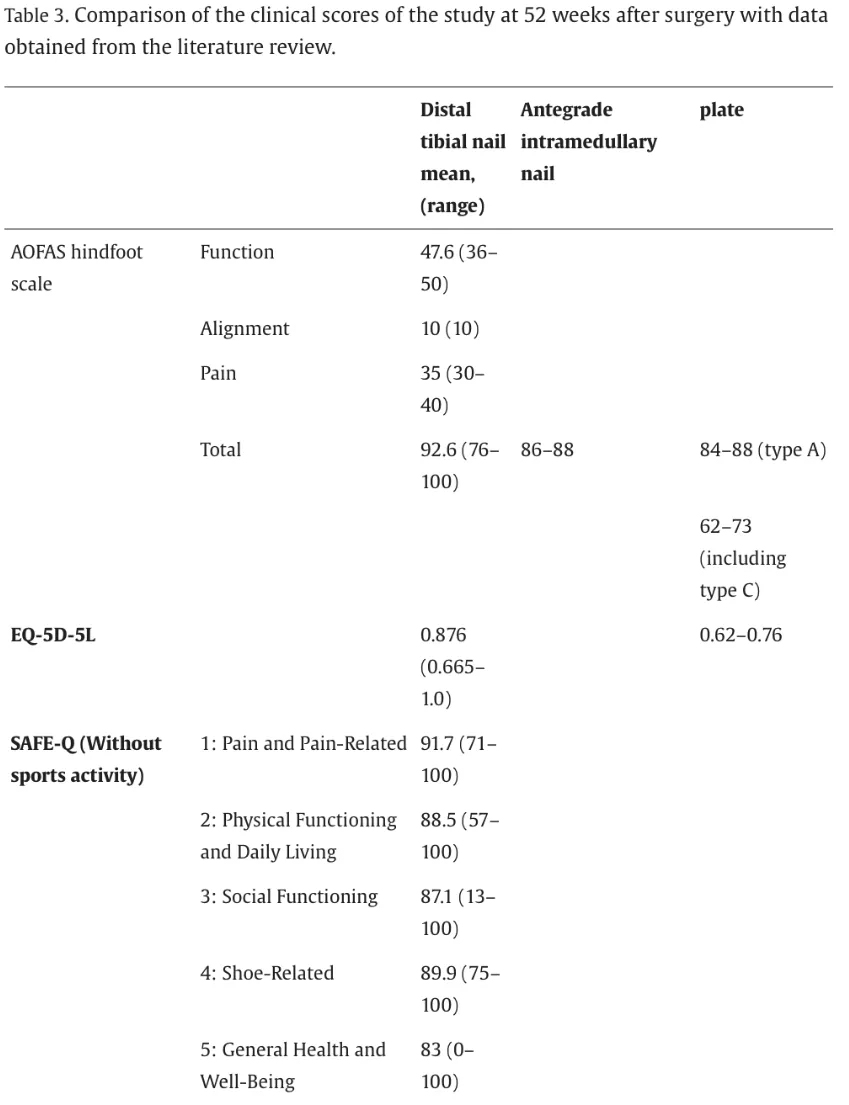
The nonunion and malalignment rates for antegrade nails are 0–25% and 8.3–50%, respectively; for locking plates, 0–17% and 0–17%. In this study, all cases achieved union, and only 20% had deformity >5°, comparable to traditional methods.Infection rates: superficial infection is 0–8.3% for antegrade nails and 0–23% for locking plates; deep infection is 0–23% and 0–8.3%, respectively. This study reported no soft tissue complications, outperforming both alternatives.Functional scores:
AOFAS scores for antegrade nails: 86–88 (type A), 73 (type C); locking plates: 84–88 (type A)
This study: AOFAS average: 92.6
EQ-5D-5L: Locking plates: 0.62–0.76; this study: 0.876
SAFE-Q (foot and ankle patients): 67–75; this study: 83–91.7 (Table 3)
Union rate, deformity rate, and infection rate outperform traditional methods
Functional scores (AOFAS, EQ-5D-5L, SAFE-Q) show excellent results
In summary, DTN offers advantages over locking plates and antegrade intramedullary nails and represents an effective solution for treating distal tibial fractures.
DTN features minimal invasiveness, high stability, and rapid recovery
It is a valuable alternative to traditional treatments and worth promoting
Yamakawa Y, Uehara T, Shigemoto K, et al. Preliminary results of stabilization of far distal tibia fractures with the distal tibial nail: a prospective, multicenter case series study[J]. Injury, 2024: 111634.
创伤骨科智能科技 智汇骨. (2024年12月31日). 胫骨远端髓内钉突破胫骨远端骨折的治疗 [微信公众号文章]. 创伤骨科智能科技 智汇骨. https://mp.weixin.qq.com/s/9UqQvJ0eAe4bKZg2U4nQ8Q (Accessed: 2025年06月07日)